The silence of deserted city streets is punctuated by the sirens of ambulances. Almost everyone in India has had a family member or friend infected by SARS-CoV-2 or with the Covid-19 disease. There are more sick people inside and outside hospitals than can be provided care by the facilities available. Doctors and nurses are overworked and stressed. There is a shortage of everything that is needed: testing kits, isolation beds, intensive care units (ICU) beds, ventilators, medicines, and medical oxygen. Even space in crematoria and cemeteries is not available.
It will be difficult to forget April 2021.
It was only on 7 March that India's health minister had announced that country was in the “endgame” against the pandemic. In early 2021, the situation of Covid-19 in India appeared under control. The country had launched its Covid-19 vaccination drive on 16 January. The political discourse encouraged talk of an ‘Indian exceptionalism’ to the experience worldwide of the virus bringing the best health services and systems to their knees. The Economic Survey (2020-21), presented in Parliament at the end of January, speculated that “the prospect of India having strong second wave is receding.” At global fora and within the country, the political leadership started taking credit for effective handling of the pandemic 1 This is in stark contrast when in the first wave, when cases spiked politicians and policymakers were quick to float the narrative of ‘irresponsible citizen’, by blaming the people for not following Covid-19 appropriate behaviour. This convenient narrative in many senses shifted the responsibility (to fight the virus) to the people as if the government had done everything needed. and even discussed what the world could learn from India.
Less than a month after the health minister’s declaration that we were in the “endgame”, India found itself in the middle of a ferocious second wave of Covid-19.
Political rallies swelled in the states going to the polls. State government advertisements invited people to the Kumbh Mela. With such statements and actions of politicians, people saw an opportunity to venture out after the restrictions of the past several months. There were large crowds in public places, malls, restaurants, and cinema halls. The use of masks declined. When they were used, masks were improperly placed, either not covering both nose and mouth or placed below the chin.
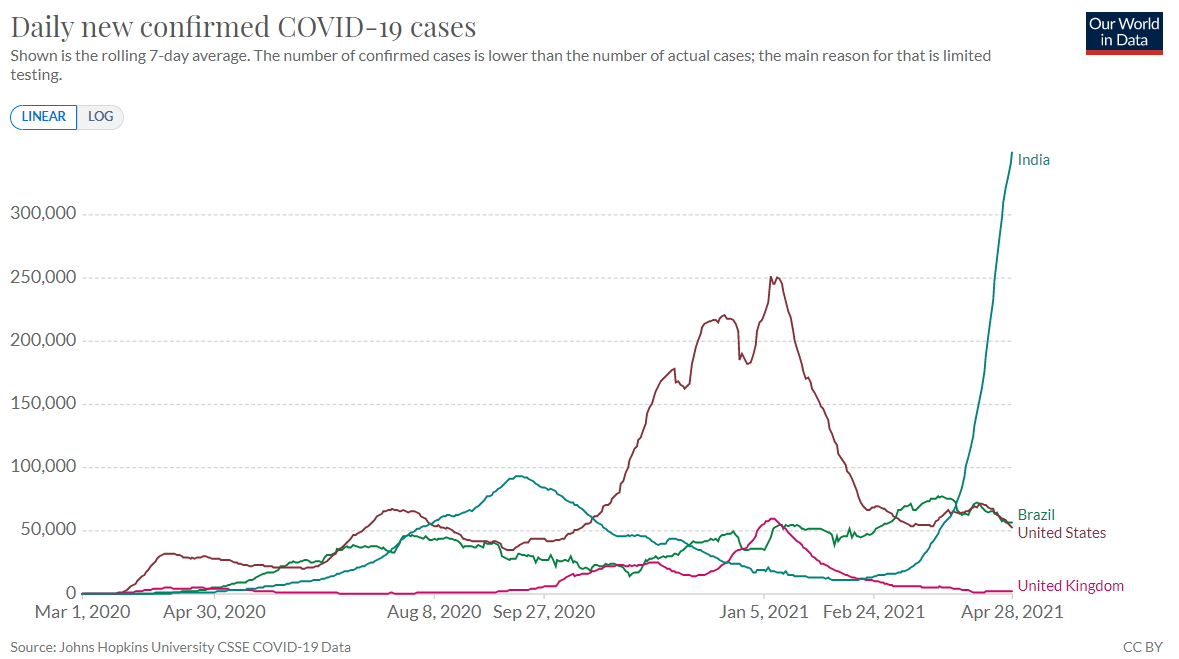
There was no reason to believe that the virus had gone away. By early 2021, several countries in the world had faced second and third waves, nearly all of which were bigger than the first. Some of them were under fresh lockdowns and other restrictions. Experts who had studied epidemics and pandemics knew that subsequent waves of the virus could not be ruled out in India, except that it was difficult to predict their timing and size.
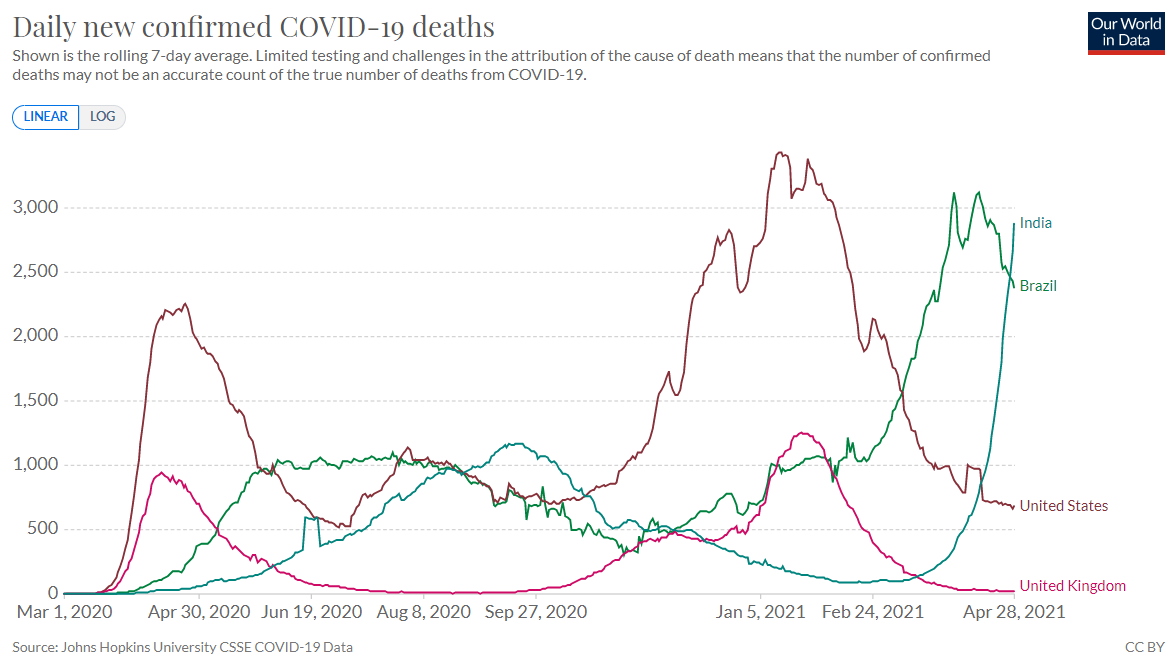
Less than a month after the health minister’s declaration that we were in the “endgame,” India found itself in the middle of a ferocious second wave of Covid-19. By mid-April India had achieved the dubious distinction of recording the highest daily cases reported thus far by any country since the start of the pandemic, with more than 350,000 new cases daily. The number of deaths also crossed 3,000 a day. The number of active Covid-19 cases in India at end April stands at over 3 million, three-fold higher than the active cases at peak of the first wave in September 2020.
‘Band-aid’ solutions and lack of planning
The Indian health system has suffered because of the approach of providing ‘band-aid’ solutions: fixing only the immediate problem and not addressing deeper maladies. Even the heightened political attention that Covid-19 received in 2020 could not result in a strengthening of the health system.
A characteristic of the response to the pandemic was the lack of planning and coordinated action […] Decision-making, mostly centralised in the political leadership, often had a semblance of being ‘ad-hoc’.
One of the stated purposes of the 2020 lockdown, by some accounts the strictest in the world, was to reinforce the health systems in India. Public health experts were pleased to hear top Indian leaders and policymakers refer to plans to do so. Yet what came, while helpful to respond to the pandemic, did not include more sustainable solutions that would strengthen the system. 2 Health system strengthening would mean actions on multiple fronts such as increased and sustained financial allocation, change in the rules and guidelines to facilitate the recruitment and retain the workforce, filling the vacancies at government health facilities; regularly train and retrain health staff in running these equipments; improved and assured provision of clinical and diagnostic services; assured supply of drugs, diagnostics, vaccines and other supplies; improving health information system and data recording and reporting; improvements in health governance including policy formulation and healthcare regulation, amongst many other aspects in sustainable manner (See Lahariya, Kang, and Guleria 2020) The initiatives taken in 2020 were to increase the availability of Covid-19 testing kits and centres, personal protective equipment (PPE) kits, N-95 masks, and isolation and treatment beds. Beds were increased by repurposing existing hospital beds as well as by converting hotel rooms and banquet halls into Covid-19 facilities.
But even these temporary facilities were dismantled by February 2021 on the assumption that Covid-19 had gone away.
The response to the pandemic has been marked by a lack of planning and coordinated action. There were no formal plans and strategies drawn up on dealing with the pandemic, on vaccination roll-out and scale-up, and on to tackling future waves of the pandemic. (If they exist at all, they are not in the public domain.)
Though several formal decision-making mechanisms were established — one each for political leaders, government policymakers, and technical health experts —these groups largely functioned independently of each other. Expert group meetings were infrequent, had limited participation of independent experts, and their deliberations did not seem to inform decisions taken by the political leadership.
Decision-making, mostly centralised in the political leadership, thus often had a semblance of being ad-hoc. Take, for example, when in the second week of April 2021, a senior bureaucrat argued why Covid-19 vaccination should not be opened to all adults. A few days later, amidst the reports of vaccine shortage and with no plans about how vaccine supplies would be ensured, the government opened vaccination to all adult citizens.
Similarly, one of the empowered groups in NITI Aayog (constituted in April 2020) and a sub-committee in the Ministry of Health and Family Welfare (formed in August 2020), were responsible to plan the supply of medical oxygen in India. Yet, eight months later the country was caught ill-prepared for an oxygen emergency.
The way forward
April 2021 has been harsh on the people of India. There is no choice but to respond to the pandemic together, effectively and promptly.
An increased engagement of independent subject experts in various technical committees and decision-making groups should be the first step. This is not a time for fault finding. However, independent voices can ensure that the right thing to be done, rather than what seems politically correct, is communicated without fear to those in power making decisions.
It is time to objectively review and implement policies that have not been carried out so far. If they are not implemented even after the biggest health crisis in independent India, then when will we act?
Both union and state governments must prepare detailed action plans to respond to the pandemic in the short term (three months) and medium term (one year). Understandably, the short-term plan has to focus on tackling the challenges at hand: hospital bed availability, oxygen supply, vaccine delivery, medicine and testing kit supply, and the sustainability of these interventions even when India crosses the peak of the second wave.
The medium-term plan should aim to prepare India for any subsequent waves. It should also prioritise an increased allocation for health from both the state and central governments and filling up vacancies in government health facilities, amongst other things.
The next three to 12 months should also be used to dust off all health-related political promises and the national and state-level health policies of the past two decades. It is time to objectively review and implement policies that have not been carried out so far. If they are not implemented even after the biggest health crisis in independent India, then when will we act?
The pandemic response strategy also needs to be shifted from the hospital and temporary Covid-19 facilities to the primary health centres (PHCs) and community health centres (CHCs).
Fighting the pandemic is going to be a long haul. Communication strategies need to be developed to increase the adoption of Covid-19 appropriate behaviours as well as tackle vaccine hesitancy. Their effectiveness must be monitored by regular field-based data collection. Community participation, engagement and partnerships for pandemic response need to be strengthened. Civil society organisations, resident welfare associations, and panchayats need to be engaged with to make these initiatives sustainable. The special allocation for health, made by the Fifteenth Finance Commission to the state governments and local bodies should be used for these purposes.
The pandemic response strategy also needs to be shifted from the hospital and temporary Covid-19 facilities to the primary health centres (PHCs) and community health centres (CHCs). There are around 30,000 PHCs and 6,000 CHCs across the country, each with six and 30 bed capacities respectively. However, many of these beds are not functional and utilised. Strengthening these facilities by filling staff vacancies, allocating medicines and other supplies, and making these beds functional and supplemented by oxygen cylinders, can create around 360,000 additional beds for Covid-19 patients.
Supplemented by a strengthening of the ambulance network to facilitate the timely referral of patients, this will prepare all for carrying through an effective pandemic response. Once the pandemic is over, these additional beds and facilities would meet the regular health needs of the citizen. That is exactly what is meant by a strengthening of the country's health systems.
In the weeks and months ahead, the demand for post-Covid-19 care and mental health services is likely to rise, for which greater finances must be allocated. The PHCs and CHCs could become immensely useful in providing these services too.
The vaccination strategy proposed in India is complicated to implement and there are challenges in vaccine supply.
Vaccines are the real hope against the pandemic, though not against this wave. The benefits of vaccination take a few weeks to be experienced. An individual can be considered protected, two additional weeks after receiving the completed schedule (or the second dose). 3 Depending upon which vaccine is administrated and the gap between two doses followed, an individual can be considered fully protected six to 10 weeks after the first jab. In India, two injections of Covaxin are recommended with a gap of four to six weeks and of Covishield with six to eight weeks. Therefore, the pace of vaccination should be scaled up, which will help in reducing hospital load and mortality in the months to follow.
The vaccination strategy proposed in India is complicated to implement and there are challenges in vaccine supply. The state governments need to recognise the challenges, allocate sufficient funding to procure vaccines and prepare detailed strategies for roll-out. They must not wait for this wave to pass to scale up vaccination.
Conclusions
We have witnessed in the past year that once Covid-19 cases dipped, the promises about strengthening and expanding India’s health systems were almost forgotten. We need to avoid a repeat of that situation.
We can be in a far better place by just fulfilling the promises of increasing government spending on health.
India needs to embark right now on long-term measures to strengthen the health systems. We can be in a far better place by just fulfilling the promises of increasing government spending on health to 2.5% of GDP, allocating two-thirds or more of government spending to primary healthcare services and increasing state government spending on health to 8% of the state budget, as stated in the National Health Policy 2017. The focus has to be on achieving this in the next five to seven years.
What needs to be done is well-known. We must re-examine solutions in the context of the pandemic, recommit with new timelines, and ensure high-level political commitment.
The Nobel laureate Angus Deaton in his 2013 book, The Great Escape: Health, Wealth and the Origin of Inequality, has argued that much of the social development and economic growth in Europe and other high-income countries can be attributed to learning from cholera and influenza pandemics, which led to these countries strengthening their public health services.
It is to be seen whether Indian policymakers will learn from the Covid-19 pandemic and strengthen the country’s health system. Or will we falter one more time?