In April 1975, an American epidemiologist, attached to the smallpox eradication team in India, stumbled upon an impending disaster (Naraindas, 2003). As part of a specially assembled international health corps, his job was to unearth cases of smallpox in what was dubbed as the last major hot spot of smallpox in the world: Bihar. But the site of his sudden confrontation with the disease was more the cause for alarm than the sizeable number of cases unearthed. It was Pawapuri near Nalanda and the occasion was the anniversary celebration of Mahavir.
Pawapuri drew to its Jain temple pilgrims from all over India. It transpired that smallpox had made its appearance as early as the first of January and had gone unreported due to a doctors’ strike. The consequences were unnerving as the massive turnover of pilgrims implied the disease would be carried far and wide. More were expected and scores would leave, many of whom would incubate the virus and show no immediate signs of the disease.
Pilgrimage, Panic and the Virtuoso
In its retrospective personal rendering in 1996 by Dr. Mahendra Dutta, the central government’s appraisal officer for smallpox in Bihar, the above incident had all the ingredients of high drama 1 This account is based on my conversation with him in 1996, referenced here as Dutta (1996). I believe he passed away this February in Ghaziabad. I would like to thank him for his time and warmth and offer this, in part, as a tribute to him, and people like him; and also to the vast mass of people who are out there right now, providing what are called “essential services” while the rest of us stay at home. I would also like to thank Richa Kumar, Sinjini Mukherjee and my Soc Med class for their perceptive and thoughtful comments, and the editors at The India Forum for their discerning comments, deft and diligent editing, and for graciously seeing this through. . On his arrival after the alarm had been raised by the American epidemiologist, Dutta realised that if not swiftly handled, Pawapuri was likely to be a major setback to India’s smallpox eradication programme, which had just turned the corner and was beginning to register a declining number of cases after a huge epidemic the previous May.
By the end of 1974, every household, village, or mohalla where smallpox was detected was cordoned off, its inmates impounded, ostensibly fed and compensated for loss of wage, and contacts vaccinated.
But its larger fallout in terms of tracking down all the pilgrims who had passed through the portals of Pawapuri seemed easier by comparison to what confronted Dutta at the pilgrim site. While a register of pilgrims allowed the smallpox eradication cell to telegraphically notify 150 districts about the returning pilgrims and the impending outbreaks, the eradication protocol at Pawapuri ran into rough weather.
The protocol called for an immediate cordoning of Pawapuri and its conversion into a quarantine site. The impounded pilgrims were to be rapidly vaccinated, and new arrivals could gain entry only if they allowed themselves to be vaccinated. Though each of these measures came to pass, they were none too easy.
There was a momentary stand-off as the pilgrims, in a familiar scenario, refused to be vaccinated on ostensibly religious grounds. The local superintendent of police, who was at loggerheads with the district magistrate, refused to co-operate making it difficult to throw a cordon around the village. At Dutta’s behest, the state’s chief secretary intervened in the dispute between his subordinates, and the pilgrims were persuaded to submit to vaccination through their religious head.
Having won, through Dutta’s institutional mandate and personal charisma, the co-operation of the local administration and the religious head, it was easy to orchestrate the rest. More than 1,000 volunteers from among the pilgrims were mobilised to act as vaccinators, run a community kitchen, keep vigil and get the rest to submit, without fail, to vaccination.
Pawapuri seems extraordinary, and certainly seemed so for Donald Henderson, the then chief of the global smallpox eradication unit of the World Health Organisation (WHO). But the measures outlined were played out over and over again throughout the length and breadth of the country, especially in the four endemic states of Bihar, Uttar Pradesh, West Bengal, and Madhya Pradesh. By the end of 1974, every household, village, or mohalla where smallpox was detected was cordoned off, its inmates impounded, ostensibly fed and compensated for loss of wages, and contacts vaccinated.
Pawapuri represented a complete inversion of what had been the vaccination practice since its inception. It was an offensive strategy of ‘search and destroy’ whose purpose was to ferret out Agent Pox
Pawapuri was a miniature writ large with a rider. Being a pilgrim centre it was potentially a site of dissemination, made doubly difficult by the fact that the pilgrims could take umbrage in faith to register a cohesive and cogent protest. But the methods and motives at Pawapuri were part of a larger piece, which in under six months produced a singular result in modern public health: the extirpation of smallpox.
In May 1975, India recorded its last case of smallpox. Two years later, the country was certified to be free not only of the disease but of the very virus. Since human beings were the virus’ exclusive hosts, the eradication of the disease meant that the virus had been extirpated from its ‘natural’ reservoir.
What were the measures that extirpated perhaps the most dreaded disease in the history of mankind, which killed roughly every third person who got the disease—as opposed to the coronavirus that in India seems to kill roughly just one out of every 30 infected persons? And is it possible to draw lessons from the past for the present?
From Reach to Incidence
Vaccination, inaugurated in India in 1802, was often falsely portrayed by the British as a monumental effort pitted against native prejudice (Naraindas 1998). Yet, as late as 1946, it touched only a small portion of British India. This was borne out by the fact that in 1951 India reported more than 250,000 cases of smallpox with 64,000 deaths. It was only in 1961–62 that the National Smallpox Eradication Programme was launched, in an attempt to cover the entire country through mass vaccination. As part of it, 80 percent of India’s population was vaccinated. While this reputedly had its effect, especially in the southern states, there was a recrudescence in 1967 with 80,000 cases, which was almost the same number of cases as were reported in 1963 when the programme started. Hence, what changed between 1967 and 1974 that led to the complete extirpation of the pox by 1975?
Till 1968, measures against smallpox were organised on defensive principles and concepts that could be traced to the nineteenth century. In stark contrast, Pawapuri represented a complete inversion of what had been the vaccination practice since its inception. It was an offensive strategy of ‘search and destroy’ whose purpose was to ferret out Agent Pox and railroad it— like the Americans were trying to in Vietnam to the Viet Cong — to extinction.
At the heart of the new strategy was the abandonment of the impossible dream of 100% mass vaccination. It was replaced by what retrospectively seems an equally impossible dream: an attempt to unearth each and every case of smallpox.
[For the global north,] it was far better to invest in the tropical world and make it ‘disease free’ [...] allowing the temperate world to [...] dismantle the expense and the bother of keeping vigil.
For the first time the focus was to be on the incidence of disease rather than on mere reach that mass vaccination represented. Every case, as in Pawapuri, would be unearthed, isolated, quarantined and the contacts vaccinated. But this conceptual shift and its shrewd administrative reworking did not come full-blown and ready-made.
A New Calculus and a Milestone-Zeal for Agent Pox
The eradication of smallpox was a global effort. And often the WHO and the United States’ Centers for Disease Control and Prevention (CDC) take the lion’s share of the credit. But what is less known is that the brunt of the effort, the chutzpah, and the expenditure, was borne by the Third World, and perhaps a major share of it by India.
The head of the WHO called it a two-billion-dollar gift from the third world to the first world; and not a one-off gift, but a gift given in perpetuity. According to Brilliant (1985: 134), the United States, for example, recovered its investment within 26 days of the world being free of smallpox—a rate of return that is equivalent to 1,403 percent per annum!
This calculus came from the fact that diseases in the global south were a threat to the global north even if the north was completely free of the disease. These countries, to stay ‘disease free’, had to keep vigil through ‘infectious disease radar stations’, to spot, isolate, quarantine, and vaccinate or treat what they perceived as ‘importations.’ The idea was to nip every importation in the bud before it led to that currently dreaded word ‘community transmission’—symbolised by the ‘corona graph’ that merrily putters along and then suddenly does a vertical take-off.
But keeping vigil to stay in a state of grace is an expensive proposition, which, if dismantled, can prove to be economically devastating—as we are now witnessing—apart from the human death toll. An outbreak in 1961 from a single importation cost the United Kingdom $3.6 million, while the Americans spent $150 million each year as the price for keeping vigil, according to an estimate in a WHO publication. Hence, it was far better to invest in the tropical world and make it ‘disease free’ (unlike dealing with hunger, homelessness, or unemployment, which are not contagious), thus allowing the temperate world to not only dismantle the expense and the bother of keeping vigil but also because sustaining (to use current parlance) a ‘corona wall’ may be far dicier than sustaining a Mexican or Mediterranean wall.
“Smallpox zero—point of no return!” [...] was a war cry that convulsed through India’s entire health bureaucracy and made it almost exclusively focus on smallpox.
But such tropical investments make sense only if there is a particular calculus of time. Global eradication was thus conceived as a ten-year programme, buoyed, according to Henderson, by another recent achievement: putting a man on the moon. Thus, a calculus of costs, predicated on a calculus of time, was wedded to achieving a mythic milestone: extirpating the pox and thus doing something—like the man on the moon—that had never been done before.
If the physicist Robert Oppenheimer, hero of Los Alamos, was responsible for a quarter million deaths in Hiroshima and Nagasaki, Henderson the epidemiologist —awarded the US Presidential Medal of Freedom in 2002—perhaps saw himself as saving half a million lives every year. But if we use ‘Henderson’ as a titular term of a discursive practice, we can see that most people, especially those who participated in what came to called the Intensified Campaign (1973–75), were fired by a kind of milestone-zeal. They saw the campaign as a charismatic and redemptive adventure that would deliver a few hundred-thousand people from death every year, and a few million more from the hideous after-effects of smallpox.
Mahendra Dutta, with his virtuoso performance at Pawapuri, was a prime example of this zeal, which in its last stages was called “Smallpox zero—point of no return”. It was a war cry that convulsed through India’s entire health bureaucracy and made it almost exclusively focus on smallpox. The Indian state’s monumental resources, and those of every person participating in it (like the 1,000 volunteers at Pawapuri), were put to do whatever it took to get over the finishing line and declare India—and thus the world—to be in a state of grace.
But this grand operative ballet – enacted against the backdrop of Jayaprakash Narayan’s civil disobedience movement, and haunted by Oppenheimer’s ghostly legacy through the detonation of a nuclear bomb at Pokharan in May 1974 – was one that required thousands of people to work together with fervour and commitment, in quite the same way that the Fat Man and the Little Boy were produced at a frenetic pace by thousands working together at Los Alamos: the latter to bring redemption through mass death; and the former to put an end to mass death by ridding the earth of a scourge.
An Atlas, a Corps, and an Image
Around 1973, the WHO borrowed William Foege from the CDC and shipped him to India to join the effort of globally eradicating smallpox. Foege, who also went on to win the Presidential Medal of Freedom in 2012, was credited with having stamped out smallpox in Nigeria. He had invented a new way of tackling smallpox under conditions of vaccine scarcity. Based on that experience, he drew up a new atlas of smallpox in India. It was an aspirational atlas that reconceived India as America.
Perhaps the most important in the new scheme of things was the raising of a select band of highly committed volunteers, who were ready to ceaselessly search for Agent Pox and thwart him.
Much to his surprise, Foege had found that vast parts of India, especially the southern states, were largely free of smallpox. Hence, he suggested that rather than seeing India as a third-world country where smallpox was endemic, it was better to conceive it as a largely smallpox-free country with pockets of smallpox (Foege 1975). The new atlas not only showed large parts of India to be smallpox free, but also allowed one to operate with the same kind of response structure that the first world operated with vis a vis the third world, which rested cardinally on seeing every case as an importation that would result in quarantine, contact tracing, and vaccination. If mass vaccination was an attempt to distribute water equally to an imagined fire everywhere, the new atlas showed the actual places on fire—the hot spots—and thus allowed one to concentrate scarce resources where they were most needed.
But what were these resources? While the obvious ones were a stable vaccine, a new instrument (the bifurcated needle), and a new technique that was quick and painless, there were several others that were needed to make the campaign a success. Perhaps the most important in the new scheme of things was the raising of a select band of highly committed volunteers, who were ready to ceaselessly search for Agent Pox and thwart him from his insurrectionary dreams.
This would be the task of Dr. R N Basu, the head of India’s smallpox eradication programme. Around the same time as it got Foege to India, the WHO persuaded Basu to spend time with a group of US Peace Corps volunteers in Ethiopia to see how smallpox eradication measures were being handled there. Basu’s time in Ethiopia, where each person, at great personal discomfort, ceaselessly criss-crossed the countryside in jeeps looking for Agent Pox, had left an indelible mark on him. It was the very antithesis of the ossified bureaucracy that he was used to.
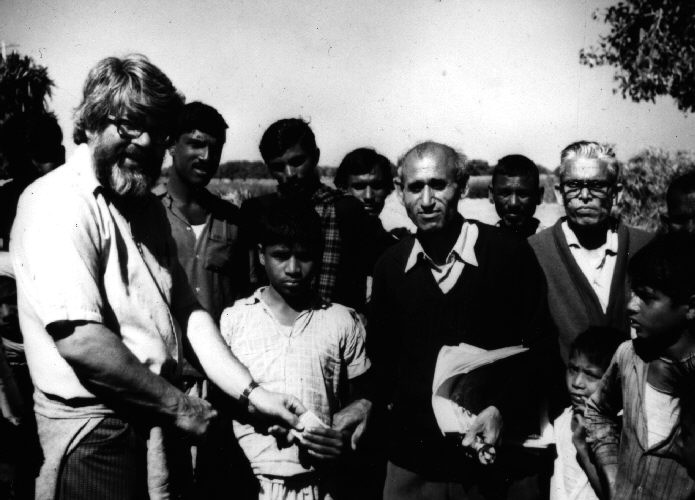
In an interview in 1996, Basu recalled that he offered to raise one Indian volunteer for every one the WHO raised. The WHO, he said, began by raising 20 that he matched. This international corps, which grew over time and became a rotating one, spent roughly three months at a stretch in the field. They were given a quick orientation, with the most productive and the longest part being the one with the sociologists, who gave them—especially the foreign volunteers—a crash course on local mores and customs that would be cardinal if the experiment was going to work (Dutta and Foege 2004).
The volunteers—or “commando units” as Basu described them—were then despatched in a jeep with a driver, a paramedic with needles and vaccine, and a comprehensive search protocol, along with a picture of a pox patient overrun with pustules. This image of Agent Pox, which they constantly carried with them like it was their new-found love and shown to all and sundry in their designated beat, was an invitation to confess.
Given the long history of a capricious state, post-colonial subjects, especially the rural poor, were wary, to say the least. Hence, as an incentive, every person who confessed to having seen Agent Pox was given 100 rupees each. Soon after, perhaps to ensure that the confessor was not seen as an informer who had ratted, the victim too was given the same sum of money, which steadily grew as the cases fell, to 1,000 rupees. This grand public confessional, goading everyone through entreaty and threat, to rise from a state of fall to one of grace, was a cardinal but not the last step in the scheme of things.
The Imprest, the Community, and the Rumour Register
Mahendra Dutta and his charismatic troubleshooting, Basu and his zealous voluntary corps, and Foege’s new atlas readily suggest themselves as new conceptual tools that redrew set procedures and ways of acting and thinking. But one normally does not think of financial instruments, especially seemingly small amounts of petty cash like the imprest, as being decisive. As we will presently see, Basu’s commando units would have been crippled without it.
[The programme’s innovations] allowed local youth to be trained as vaccinators in “twenty minutes” and to create a “containment ring” by tracing and vaccinating all contacts.
“We were, […] apart from the Jeep, the paramedic, the medical supplies, and the driver, given a generous imprest and allowed to spend it as we saw fit,” I C Tiwari recalled in an interview in 1996. Posted as a senior epidemiologist with the voluntary corps in Champaran, Bihar, Tiwari had to ferret out Agent Pox against the backdrop of the Indian state combating the Naxalite insurgency of the time.
The Naxalite insurrection, among other things, disallowed night-time travel and hence speed was of the essence for the volunteers. Tiwari could use the imprest to replace the vaccine, change the tyres of his jeep, or hire local enumerators and vaccinators on the spot to get the job done. His choice of examples was all suggestive of pace: replenish used-up vaccine or swap used-up tyres; get village youth to act as enumerators, stand guard, or run a community kitchen; or quickly hire them to double-up as vaccinators.
All of these became increasingly important as sometimes there were deaths after a post-infection vaccination. When cases had been found, one had to work with great pace to get the job done before there was a death. It could break community confidence and derail the exercise. Hence the seemingly humble imprest, and the flexibility it provided, was the key.
But so was the rediscovery, given the size and scale of the operation, of the village as hallowed space and the community as coparceners in the eradication of the Pox. The community had to confess, albeit with incentives. Having done so, it had to agree to not merely passively cooperate but be actively enlisted, for a nominal fee, in getting the job done. This was fortunately enabled by the introduction of a new freeze-dried vaccine that was stable unlike the earlier liquid vaccine, and the arrival of the bifurcated needle in lieu of the painful and cumbersome rotary lancet.
These innovations, said Tiwari, allowed local youth to be trained as vaccinators in “twenty minutes” and to create a “containment ring” by tracing and vaccinating all contacts. And the ring grew in size as the cases fell, in quite the same way that the reward for confessing grew from one hundred to one thousand rupees each as the cases became few and far between.
But the flexible financial instrument of the imprest, so cardinal in ‘getting the job done,’ and the re-inscribing of the village and the community as instrumental to the search and containment protocol, were only possible because of a continuous refinement in the search protocol. Its acme was the rumour register that served several functions at once.
[C]onceptual refinements, and an esprit de corps, spurred in the final stages by the attraction of achieving a historic milestone, corralled Agent Pox, by inches, into extinction.
Smallpox was part of a family of exanthematous diseases marked by fever and rash, with its closest sibling being chicken pox. To ensure that no cases were missed, all cases of fever and rash were entered in a rumour register in an initial search. Tiwari’s job was to start the day by looking at the rumour register and then setting out to confirm whether the cases were smallpox. This act of confirming the rumour became a second-order search and allowed the programme to finesse the search and containment protocol.
Finally, when all the district-level data from the rumour registers was collated, if it was found that there was a “nil” district sandwiched between two districts with high incidence of fever and rash, the programme knew that there was something wrong. The corps would swing into action to investigate the anomaly. It invariably unearthed fudging, either due to ‘target pressure’ or corruption. This was set right by often easing personnel who operated in a business-as-usual mode to other departments, and by meticulously going through the rigmarole of search, segregate, quarantine and containment by ring vaccination in the “nil district.”
These conceptual refinements and an esprit de corps, spurred in the final stages by the attraction of achieving a historic milestone, corralled Agent Pox, inch by inch, into extinction.
The Hiatus between Person and Disease: Rendering Recalcitrant Bodies Inert
In 1665, the appearance of plague in London resulted in the opposite of Passover. The red mark on the door of plague households was a sign, not for god to pass over and spare their first-borns, but to seal and condemn its inmates to death. While we can assume with reasonable certainty that the plague in 1665 announced itself with fever and chills, and with the characteristic swelling of the lymph nodes, we are now saddled—starting nominally in 1800 with the advent of histology—with a paradox peculiar to modern medicine: the possibility of disease without a patient; and of patients with no disease (Naraindas 2006, 2011).
The asymptomatic Corona infectee—10 to 30 percent of total infectees, according to different estimates—is the perfect example of the presence of disease in the absence of the patient. On becoming infected, they, like other infectees, presumably incubate the virus. But instead of exhibiting symptoms and becoming patients, they become asymptomatic carriers of the virus and silently spread the disease.
In the currently bigoted landscape, [asymptomatic infection] unfortunately makes already suspect bodies hyper-suspect and, as is currently the case, weaponises them as veritable corona-bombs on an insurrectionary run.
What flows from this cardinal epistemic premise (not shared by other systems of medicine) is that these persons are merely a detour to the virus. Neither their experience nor their testimony (of feeling fine, for example) necessarily counts as evidence. And if they are not willing to come forward and follow the rules laid down to ferret out Agent Corona, who they may be secretly harbouring in their person, they are committing treason against the commonweal (Naraindas 1998).
In the currently bigoted landscape, this unfortunately makes already suspect bodies hyper-suspect and, as is currently the case, weaponises them as veritable corona-bombs on an insurrectionary run; while the bodies of the poor are made into expendable collateral.
Simulated war games and movie scripts of contagious or infectious diseases are often predicated on both of the above. The viewer’s sense of impending doom is marshalled, either through a pet monkey carrying the Ebola-like virus from Congo to California in the movie Outbreak, or as a ‘terrorist’ incubating the smallpox virus and carrying it on his person to either Heathrow or O’Hare, and deliberately spreading it by walking around the airport, before curling up in a corner to die as a ‘martyr to a cause.’ While this provides such plots their initial insurrectionary impetus, the plot culminates in Outbreak with an unthinkable collateral: the possibility of nuking an entire lily-white American town to contain the virus. This is of course prevented at the last minute, unlike the ready and easy expending of an African village as collateral at the beginning of the movie. But in a retributory move for this original sin, a virus-infected-monkey escapes the nuking, and comes home to roost.
The Epidemic Diseases Act of 1897, first put into play with great alacrity in Bhilwara, Rajasthan, was invoked on behalf of Agent Corona and his insurrectionary run, in an attempt to hunt him down and corral him. And the searching, testing, segregating, sealing, and quarantining were all done, and are now being done throughout India —and the world—to railroad him into extinction.
This singular focus on Agent Corona as the causa causans valorises the virus and leads to an imagery of war, and concomitantly leads to a hiatus between the disease and the person, especially the carrier. Hence, it is none too surprising that Ludwick Fleck (1935), soon after the microbe had ascended to being the principal dramatis persona, called it the devil re-incarnate. An ontological point of view that affords us, as Canguilhem (1978) points out, a soothing certitude of a Being against which one can do battle.
Thousands of posters were printed depicting smallpox as a pox-ridden cross between a horned devil and an ear-ringed rakshasa, who was down but not out [... and impaled] with the bifurcated needle.
Our rendering unsurprisingly follows the above trajectory, and the virus’ singular agency is hypostatised and anthropomorphised by the epithet of Agent Pox or Agent Corona, as it effortlessly suggests itself by the modalities put into play to address its seemingly insurrectionary potential. This is buttressed by the fact that the Intensified Campaign was coeval in time to the Vietnam war where the Viet Cong were also (if not principally, as that war was costlier in terms of men and money) caught up in an insurrectionary template, and the American way of dealing with them was through ‘Search and Destroy’.
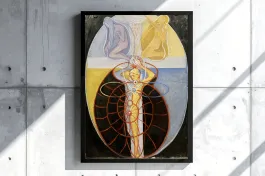
Such transpositions and anthropomorphisms, from a theatre of war to a theatre of disease eradication and vice versa, are quite common. This, in fact, was the final rhetorical move of the Intensified Campaign in 1974 and became de rigueur towards its end. Thousands of posters were printed depicting smallpox as a pox-ridden cross between a horned devil and an ear-ringed rakshasa, who was down but not out. This creolised image, understandably, was impaled neither with a trishul nor by a goddess (like the asura was by Durga and her trident), but with the bifurcated needle that looked like a trishul, and by a man in underwear who looked like a wrestler from a rural akhara (wrestling academy).
This rhetorical move located the image in a rural landscape and in the realm of human possibility and science, playing all along on a readily available divine template of the smallpox goddess Sitala Mata and her understudy Jwarasur, the fever demon, but with a cardinal difference. While smallpox under the sign of Sitala led to a mode of sequestering the patient by consecrating him, as he was the repository of the deity who would leave if a regimen and a quarantine was strictly followed (Naraindas 2003a), in the new scheme of things smallpox was seen as a demon located in recalcitrant bodies that needed to be rendered inert—by vaccinating them—for the sake of public welfare.
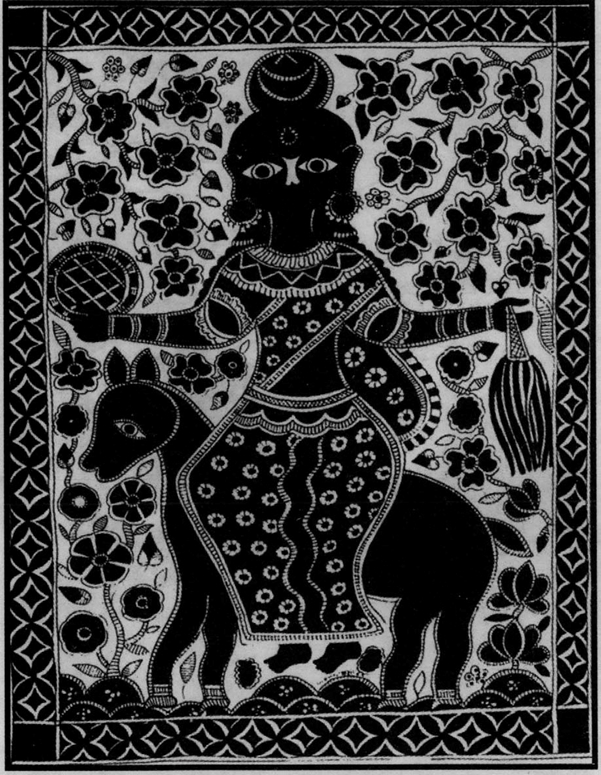
But this could not be done without ‘local participation,’ given the magnitude of the problem. Hence the village had to be re-inscribed as ‘hallowed space’ and the ‘community’ had to be enlisted as coparceners. And the poster with its creolised image was a rhetorical move that attempted to signal the rural as a ‘newfound arcadia’, whose ‘local youth’, quickly trained in ‘twenty minutes’ to be vaccinators, would be the neophytes who would wage war and impale the Devil-Rakshasa with the bifurcated needle/trishul.
If there was collective resistance—which did happen in a tribal village, which unlike Pawapuri could not be persuaded—the state would seal it with a cordon sanitaire and the disease would be allowed to smoulder and die. And the two thirds of the persons who survived the disease – given smallpox’s case-fatality ratio of 30 percent – would be presumed to be both immune and inert – and hence no longer a public threat.
Coda: From an Imagery of the Kill to a Community of Coparceners?
Since this is being written in the middle of the coronavirus pandemic, we end by highlighting some possible differences—since the parallels are evident—between the past and the present. Although Covid-19 started as a sub-tropical epidemic in Wuhan, unlike other post-war epidemics, it did not stay true to form and move south toward the tropics. Rather, it moved north to what is now being dubbed as the (in)temperate world of ‘promiscuous passports,’ and became a full-blown pandemic.
[T]here are likely to be several moves in India that are eerily reminiscent of smallpox.
If we go by Event 201, the eerily prescient simulation run at Johns Hopkins University in October 2019, Covid-19 may well run for 18 months with 65 million deaths—though there seem to be kinder ‘predictions’ lately from the US Department of Homeland Security. It will ostensibly ebb when 60 to 70 percent of the global population has been exposed to the virus. Unless old drugs, a re-purposed cocktail of drugs, or repurposed vaccinations like BCG, or plasma from recovered patients, or other novel therapies step in, surprise us, and save the day.
In the absence of these, there are likely to be several moves in India that are eerily reminiscent of smallpox, with the large-scale incarceration and hosing down of the poor and the migrant with chemical disinfectants as its exemplary form; and charging clerics with culpable homicide for spreading the virus its sinister and contemporary variant.
Such moves, apart from being inhumane, are likely to be counterproductive and may come back to bite not merely the well-to-do and the bigots, but the whole country. The Ministry of Health and Family Welfare has woken up to the first possibility and has issued an advisory saying that hosing down persons (read the poor) with chemical disinfectants is not advisable, as it is (a) harmful, (b) not effective and (c) leads to a false sense of security and may detract persons from practicing either social distancing or hand hygiene.
Unfortunately, other than some muted remarks by a joint secretary, no such clear and unambiguous directive has been issued by the health ministry saying that demonising religious or ethnic minorities could (a) actively drive Agent Corona underground and thus help spread the infection, (b) sustain the infection for much longer, and (c) delay the exit from the lockdown.
But perhaps the most important, if India is to succeed and not have more deaths from the effects of the unprecedented global lockdown that has quarantined the earth, may be to socialise and rediscover the village and communities as coparceners in this war, albeit in ways different from smallpox, which had cleverly “enlisted” them on behalf of the vaccine.
India may have to soon find ways in which people at large, and rural peoples in particular, may be counted as knowledgeable citizens and coparceners, rather than as recalcitrant body population
We have already witnessed, albeit in limited ways, a concerted socialised response across sectors, such as the temporary nationalising of private hospitals, hotels and other public institutions for an impending quarantine, the setting up of homeless shelters and the running of community kitchens, the distribution of rations and protecting wages, providing health insurance and free testing, and getting our universities, industrial outfits and home based production units into making jugaad masks, testing kits, PPEs and ventilators.
We have also witnessed, for example, Tamil Nadu’s health secretary, Beela Rajesh, or district magistrates Adeela Abdullah in Wayanad, Kerala, and Rajendra Bhat in Bhilwara, Rajasthan, step up in amazing ways during this moment. Like Mahendra Dutta in 1974, they have brought their charisma and acumen to bear with remarkable effect on a crisis situation and have been credited for either flattening the curve or stopping the virus in its tracks.
There are hundreds of others at the lower end of the hierarchy, who are the counterparts of Adeela, Beela, and Bhat. They have not only stepped up in unsung ways, but as the actual feet on the ground, are putting their lives at risk. Many of these unsung and poorly protected frontline health workers, especially the sanitation workers, some of who may contract the virus and die trying to save the rest of us, are being either shunned or attacked by a spooked population, exacerbated by a trust deficit in an increasingly bigoted landscape where minority and marginalised groups are being continuously demonised.
But apart from these noble moves by well-intentioned persons and organs of the state, seemingly never enough and often thwarted by not just corruption but also by egregious rules, India may have to soon find ways in which people at large, and rural peoples in particular, may be counted as knowledgeable citizens and coparceners, rather than as recalcitrant body populations against whom and through whom, but always in whose name, one wages war against the virus.
If it does, the state may discover that people have their own ways of practicing a self-imposed quarantine, as was the case with smallpox and perhaps continues to be the case with chicken pox and other exanthematous diseases, which may go by other names in native disease classifications. There are already reports of villages, especially so-called ‘tribal’ ones, where modes of quarantine are being practiced by the villages on returning migrants from the cities, though in some cases this could easily turn into a kind of vigilantism.
[R]ural communities may also have ways of addressing, through their local health traditions, the so-called ‘symptoms’ of the ‘infection’ like fever and cough, including the most problematic ones.
Such aberrations apart, segregating and quarantining should not surprise us, as self-sequestering and abstinence of varying lengths, often regulated by the almanac, which functions as an agricultural, liturgical and prophylactic calendar, may continue to be the bedrock of rural life. In the absence of a vaccine, it may be cardinally necessary to draw upon such a repertoire. Especially so, if the battle against the coronavirus turns out to be a long-drawn-out one, or worse, fought every season.
Finally, along with sequestering, rural communities may also have ways of addressing, through their local health traditions, the so-called ‘symptoms’ of the ‘infection’ like fever and cough, including the most problematic: the shortness of breath and the inability to breathe. This requires oxygen and the ventilators, which India may not have enough of if the plot gets out of hand. But this may be possible only if we are open to the idea that local health traditions may be able to conceive of the present distemper in their own ways, and translate the Covid-19 symptoms into ‘disease entities’ and ‘treatment protocols’ of their own.
The fact that this may be already afoot, in an attempt to enfold the novel into the familiar, is the making of papier mâché coronavirus masks of Jharkhand. Borrowed from the idiom of the Chau dance, this mask comes with a three-ply fabric encased, thus making it a Chau-coronavirus mask. This allows the mask makers to continue their tradition, and contribute an indigenous and colourful item towards the much-needed personal protective equipment. But most importantly, it allows them to continue to making a living in an idiom that is wholly their own. Perhaps in the next season they will incorporate the mask into their performance repertoire, where the coronavirus metamorphoses into Coronasur, like Jwarasur the fever demon, to be either impaled or cast out. By doing so they may, as has been case with smallpox and other epidemic diseases in the past, convert calamity into community, and transpose the historical into the mythical to edify transcendental truths.