These testimonies from patients were reported in an empirical study on how private hospitals in Maharashtra responded to the state-imposed regulation on rates for treating those suffering from Covid-19. The experiences of Covid-19 patients treated in the state’s private hospitals illustrated how multiple tactics and excuses were employed to not comply with what the government had prescribed so that the sick could be fleeced.
Background to the Study
In response to the public health emergency of the Covid-19 pandemic, the Maharashtra government was forced to take some unprecedented policy decisions on how the private healthcare sector handled it. The government had to rely on the private sector to expand its capacity to provide health services but it also had to intervene when there were widespread reports of excessive billing for treating Covid-19 patients in private hospitals.
While the decision to regulate rates was quite significant, its implementation faced multiple challenges.
Many private hospitals in India, especially corporate ones, saw the pandemic as an opportunity to maximise profits, as widely reported in the media. Some Covid-19 patients were reportedly charged Rs. 50,000 to Rs. 1 lakh a day for treatment. A major corporate hospital in Delhi set its rate at Rs. 72,500 a day for treatment in an intensive care unit (ICU) with ventilator support.
To prevent price gouging by private hospitals, many state governments regulated the rates they could charge for Covid-19 treatment. Fifteen of them directed private hospitals to reserve 20% to 80% of their beds for Covid-19 patients, invoking generic emergency provisions such as the Disaster Management Act (DMA) and the Epidemic Diseases Act.
Maharashtra was the first state to do so in April 2020. While the decision to regulate rates was quite significant, its implementation faced multiple challenges.
We conducted a study to examine its implementation in Maharashtra, which regulated rates for 80% of the beds in private hospitals. In-depth interviews were conducted with 100 Covid-19 patients who had been hospitalised, their relatives, and 12 stakeholders, including medical practitioners, state officials, and civil society representatives between November 2021 and February 2022.
The respondents were identified through referrals from two large voluntary networks in Maharashtra, which were active in Covid-19 relief work—the Corona Ekal Mahila Punarvasan Samiti and the Jan Arogya Abhiyan. Respondents were selected using a set of criteria, including complaints of excessive charges, the availability of medical bills, and their willingness to share experiences and documents. All the 100 respondents came from 15 of the 37 districts in Maharashtra, and a bill-by-bill analysis for 120 hospitalisation episodes (some patients were admitted to more than one private hospital) was carried out.
Most Hospitals Evaded Regulation
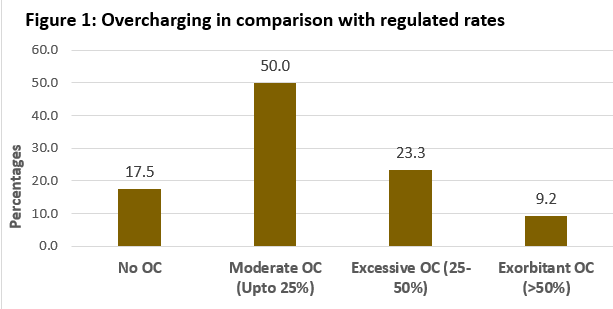
The bill-by-bill comparative analysis (n=120) against the benchmark of official rates for Covid-19 packages showed 82.5% of hospitalisation episodes involved overcharging (Figure 1). While all types of hospitals exhibited excess charging, large hospitals did it at a higher frequency and scale than medium and small ones.
Further, an analysis of per day expenditures for hospitalisation and medicines for a subset of 77 Covid-19 critical care episodes revealed average daily medical bills were 400% to 500% higher than what the expenses should have been according to official rates. This showed that the regulations did not have the desired impact of keeping medical bills affordable to all.
Double Charging
Most private hospitals used diverse strategies to circumvent rate regulations, including charging for items already included in official packages that had been paid for. For example, if a patient was admitted to an ICU with a ventilator, the maximum daily package rate was Rs. 9,000. This included charges for the bed, doctors and specialists, and nurses as well as for the ventilator, monitor, and oxygen supply. However, many hospitals charged separately for each of these items, which resulted in a substantial inflation of bills.
Inflated Charges
A wide range of items or services were not included in the official packages. Cashing in on this, many private hospitals charged exorbitantly for them. This included medicines, diagnostic and other procedures, and equipment and biosafety material.
In the name of observing Covid-19 protocols, some hospitals charged unreasonably for PPE kits. Some patients even reported they were charged for three to four PPE kits a day. For 40 patients, the total PPE bill ranged from Rs. 9,000 to Rs. 72,500. On top of this, 66 of the 100 patients had to pay more than Rs. 100,000 for medicines.
Since there was no explicit mention of PPE in the official packages, hospitals exploited it to make profits. As a doctor from a medium-scale hospital observed, “The Covid-19 pandemic was an opportunity for the medical fraternity to regain patients’ trust. Barring a few exceptions, most doctors and hospitals missed this opportunity.”
Irregularities in Billing
Non-itemised billing was also used as a way to evade the cap on hospital rates. Irregularities such as handwritten bills, false bills, and other non-transparent methods were reported by the respondents. Most private hospitals did not issue itemised bills. For example, a patient was charged Rs 1.5 lakh for a specialist’s visit during 19 days of hospitalisation.
In … [one] case, when a proper bill was asked for, the doctor responded, “I was the only one who agreed to admit you. So, you should be thankful to me rather than asking for papers and bills!”
Some patients were falsely charged for services they did not use such as oxygen, ventilators, ICU, mineral water, and so on. Some respondents reported having received handwritten bills for amounts as large as Rs. 200,000. In another case, when a proper bill was asked for, the doctor responded, “I was the only one who agreed to admit you. So, you should be thankful to me rather than asking for papers and bills!”
Such instances demonstrate the struggle patients had to just obtain proper bills and point to the need for the authorities to standardise billing formats in all private hospitals in the country.
Limited Impact
The pandemic became the policy window for reactivating the hitherto stalled agenda of implementing rate regulations in private hospitals. Growing complaints by the people and the demands raised by civil society groups resulted in the emergence of a political will to impose Covid-specific regulations on private hospitals.
However, state regulatory measures faltered in implementation and could not act as an effective deterrent against excessive charging by most private hospitals. The effectiveness of regulatory measures seemed to be severely impeded by issues where the three actors—the state, private hospitals, and patients—intersected.
One, there was the background of rampant commercialisation of the private sector, a lack of transparency and not using standard formats for billing. Two, there was the pre-existing lack of a larger regulatory mechanism over the private sector. Instead, there was only the practice of declaring impromptu regulation using the weak legal instrument of the Disaster Management Act.
Three, the states did not have the regulatory capacity to monitor the implementation of regulations, and gaps in the rate packages provided hospitals with an opportunity to issue high bills. Four, the knowledge asymmetry between doctors and patients led to medical expertise-based financial exploitation of patients.
Nevertheless, the Covid-19 regulations offered critical lessons for regulating private sector hospitals in the future. The limited success the impromptu and enforced regulation had during the pandemic underscores the need for robust, institutionalised frameworks to ensure social accountability of the private healthcare sector.
Shweta Marathe is a researcher at SATHI, Pune. She is currently a fellow of the India-HPSR Fellowship Cohort-2022.