The Covid-19 pandemic wreaked unprecedented havoc on the lives and livelihoods of people in India, disproportionately upending those on the margins of society. This great disaster exposed the fragility of state capacity and the inability of the country’s health system to cope with major public health challenges. The pandemic was also a serious setback to achieving the United Nation’s Sustainable Development Goals, where India ranks 121 amongst 163 countries, below all South Asian nations except Pakistan.
The country now faces a high prevalence of communicable diseases in tandem with an increasing incidence of non-communicable diseases. Decades of sub-optimal investment in healthcare, a lack of political commitment to the ideal of universal quality healthcare, and the absence of a comprehensive strategy to address the glaring inequities in health outcomes in the country are not accidental policy failures. They are structurally embedded in the political economy and socio-cultural matrix of the country, one which does not consider health, nutrition, education, and the like as public goods. There has been no political consensus, let alone social contract, on incorporating health, nutrition, education, social safety, gender, and social equality as critical inputs to economic development.
[H]ealthcare in India is provided by a range of professionals, including allopathy, and ayurveda, yoga and naturopathy, unani, siddha and homeopathy practitioners, dental surgeons, nurses, auxiliary midwives, pharmacists, paramedical professionals, accredited social health activists....
While the strategic framework for universal healthcare requires a comprehensive strategy, a consistent policy framework, political commitment, social buy-in, and community participation, the most critical ingredient is the capacity and commitment of the human resources that manage the health system. During the past two and half decades, public policies have focused almost entirely on tertiary care while expanding the private sector’s role in the delivery of healthcare. This has shrunk the workforce in the public domain, which has further debilitated the primary and secondary healthcare systems.
Inequities Galore
The World Health Organization’s (WHO) Global Strategy on Human Resources for Health – Workforce 2030 notes that “adequate investment in health workforce along with availability, accessibility, acceptability, and coverage are essential for overall social and economic development.” In a 2020 report, the WHO highlighted that India needs to achieve a minimum threshold of 44.5 health workers per 10,000 population by 2030 in order to secure universal quality health care.
Healthcare in India is provided by a range of professionals, including allopathy, and ayurveda, yoga and naturopathy, unani, siddha, and homeopathy (AYUSH) practitioners, dental surgeons, nurses, auxiliary midwives, pharmacists, paramedical professionals, accredited social health activists (ASHAs), and so on. The education and the practice of each of these categories are managed by different agencies with different skills, knowledge, and attitudes in different states and districts, which results in a vast diversity in health outcomes.
Obtaining an accurate estimate of the number of health workers in the country is a challenging task because the National Health Workforce Accounts (NHWA) are collated from different professional agencies that do not maintain live registers and do not account for death, retirement, emigration, double counting, and so on.
Yet, in terms of numbers, the country has a shortage of not only doctors, but also nurses, mid-wives, and other health professionals. India has 17.47 nurses and auxiliary nurse mid-wives (ANMs) per 10,000 population, or a total of 2,412,621 nurses and mid-wives. This can be compared to 39.54 and 31.52 nurses per 10,000 population in Indonesia and Thailand respectively. The Medical Council registers in the country list a total of 1,232,205 doctors, which means 7.76 doctors per 10,000 population (the number will be higher if AYUSH practitioners and dentists are included). In comparative terms, the figures are 11.18, 12.29, and 22.27 doctors per 10,000 people in Indonesia, Sri Lanka, and China, respectively.
States in the South and West of India, which have a third of the country’s population, have nearly half of all health professionals in the country. The rest of India has two thirds of the population but just about half of the total health personnel.
While a certain number of health professionals are a pre-requisite for delivering healthcare, it is hardly a reliable indicator of either the quality of care or health and nutrition outcomes. A rational distribution of health human resources would be based on the disease burden of different places and the ease of getting there combined with the knowledge and skills of the professionals involved. Together, this would be the best determinant of the effectiveness of the health service.
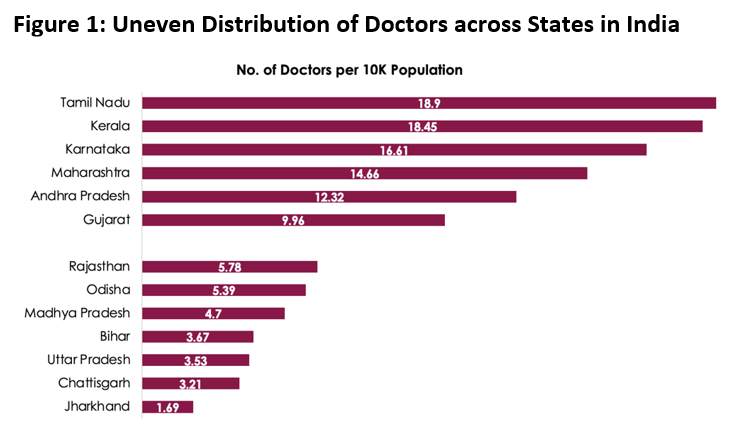
Figure 1 illustrates the seriously skewed distribution of doctors across states in India. While Tamil Nadu has 18.9 doctors per 10,000 population, Bihar and Uttar Pradesh have an average of only 3.5 doctors for the same number of people, and Jharkhand has only 1.69 doctors per 10,000 people. The situation is the same with other health professionals as well.
States in the south and west of India, which have a third of the country’s population, have nearly half of all health professionals in the country. The rest of India has two thirds of the population but just about half of the total health personnel. 1Among the states, Maharashtra has the highest number of doctors (183,843), followed by Tamil Nadu (144,737), Karnataka (126,567), and Andhra Pradesh (102,924). Karnataka has the highest number of registered dental surgeons (43,876), followed by Maharashtra (40,470), Tamil Nadu (25,183), and Andhra Pradesh (21,355). More important, nearly 65% of the health professionals are in urban areas, and the tribal areas receive only a fraction of the professional services that towns do.
Therefore, it is but natural that the gap in the professional health workforce is filled by the untrained registered medical practitioners (RMPs), traditional birth attendants, faith healers, bonesetters, pharmacy outlets, and the like, especially in rural, tribal, and urban slum areas. This gross inequity in health human resources deployment has barely been acknowledged, let alone remedied, by successive governments.
Upgrading medical education
The first medical college in India was established in 1835 at Kolkata. At the time of Independence, India had 19 medical colleges with around 1,000 MBBS seats. This increased to 143 medical colleges by 1990, mostly in the government domain. By 2021, the number of medical colleges had reached 648, with 357 in the government sphere and the remaining 291 (about 45%) in the private sector. The number of private colleges increased by 625% (from 41 to 291) between 1990 and 2021, whereas the number of government-run medical colleges increased by 250% (from 102 to 357). This was an overall growth of 343% during the post-liberalisation era.
Overall, India now has 148,042 seats a year available for various types of allopathic medical courses. Of these, the MBBS has 98,938 seats (52,123 in government colleges and 46,815 in private ones) and the MD/MS courses have 44,114 seats (25,910 in government colleges and 18,204 in private ones). The intake for super-specialist education was 9,468 in 2021. On an average, India has one medical college for every 21 lakh people and one MBBS seat per 14,000 people.
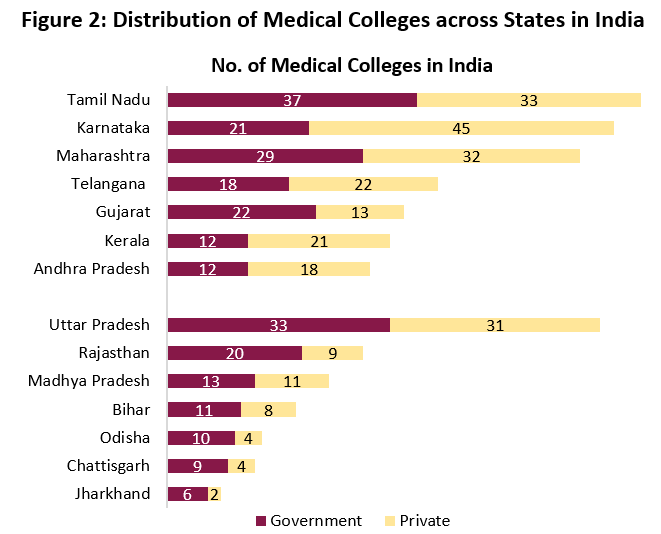
Figure 2 shows the glaring inter-state variation in the number of medical colleges and the number of seats for graduate and post-graduate medical education. It can be seen that the states having better health outcomes have a higher proportion of colleges and seats.
The five south Indian states with 20% of the country’s population have 239 medical colleges. This is 37% of the total medical colleges in the country, with 37,390 MBBS seats (38%), 16,011 post-graduate seats (36%), and 1,675 super specialist seats (34%). Of the 239 medical colleges, 138 with 22,895 MBBS seats (59%) are in the private sector.
Gujarat and Maharashtra together have 96 medical colleges with 16,320 MBBS seats. If this is added to those in the five south Indian states, the total would be more than half of all medical colleges and MBBS seats in the country.
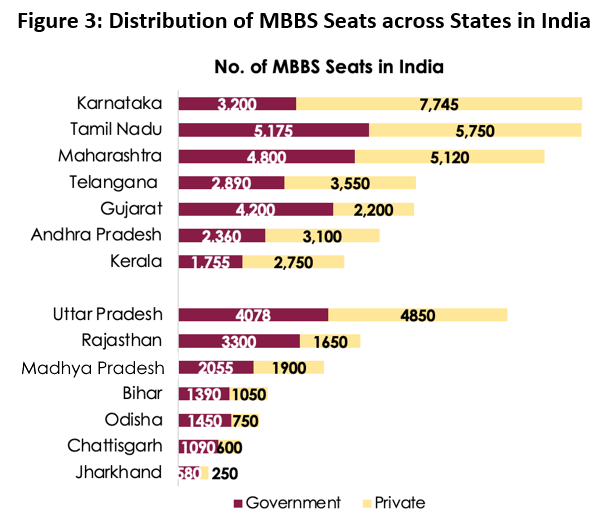
People in the states of Odisha, Madhya Pradesh, Uttar Pradesh, Jharkhand, Chhattisgarh, Rajasthan, and Bihar, who together constitute 47% of India’s population, face discouraging health outcomes. They have only 171 medical colleges, of which 69 are in the private domain, and a total 24,993 MBBS seats. This is only 25% of the total medical colleges and MBBS seats in the country. The north-eastern states and the hill states of Uttarakhand and Himachal Pradesh, which have a smaller population and more inaccessible areas, also have access to fewer medical colleges and far fewer MBBS seats than required.
Indian medical education has been almost entirely focused on the number of medical colleges and seats with little or no attention to the substantive content of MBBS training.
The southern and western states of India with a high doctor to population ratio (15 doctors per 10,000 people) have around 700,000 of the total 1.2 million doctors on the country’s Medical Council registers. The seven northern states with nearly half the country’s population have only four doctors per 10,000 population. The establishment of medical colleges and the number of MBBS seats is greatly skewed in favour of the better-off states, much to the detriment of the other states that urgently need the services of more health professionals. The current policy for admission to MBBS with state and national quotas further accentuates regional inequities.
Indian medical education has been almost entirely focused on the number of medical colleges and seats with little or no attention to the substantive content of MBBS training. Much remains to be done, including setting a curriculum and pedagogy appropriate for the Indian health context with an emphasis on promotive and preventive healthcare. There is also the issue of faculty development, and establishing outcome standards for knowledge, skills, ethics, aptitude, attitude, research, innovation, and application.
Blaming the colonial legacy for the sorry state of the health system in the country no longer carries conviction because it does not stand up to scrutiny. After World War II, the UK not only introduced the National Health System (NHS) to deliver universal healthcare, but also overhauled its medical, nursing, and paramedical education to be in sync with its goals and objectives. Such a transformation has never been considered by India for a context that is far more complex and challenging.
Medical education for whom?
The medical education strategy of the government has been “to establish new medical colleges, particularly in the private sector; increase the intake capacity of the existing institutions; and upgrade the existing district hospitals as medical colleges”. It does not even make a passing reference to the glaring inter-state inequities. The narrative touted by a few reputed doctors, who happen to lead large health corporate conglomerates, is that “the number of doctors is seriously inadequate to meet the healthcare needs of the country and government resources are inadequate to bridge the demand-supply gap”.
This premise has been the pretext for the insane rush to establish new medical colleges and increase the number of MBBS seats - with the private sector in the lead. Further, the Niti Ayog has been advocating a “rapid scale-up of MBBS seats by converting district hospitals into medical colleges using the private-public partnership (PPP) model.”
It would be naive to expect an MBBS doctor who purchased entry to a medical college at great cost to provide healthcare without extracting a reasonable return on investment.
However, increasing the number of medical colleges and seats without paying attention to inter-state inequities, intra-state disparities, the asymmetry in demand and supply, the shortage of faculty, and the lack of exposure to primary and secondary healthcare, might increase the number of doctors, but it is unlikely to make India and Indians healthier and happier.
The exponential expansion of the private sector, which is inevitably driven by the profit motive notwithstanding the “not-for-profit legal framework” of trusts, societies, Section-] 8 companies, and so on, is incapable of preparing doctors for the Indian context. They extract lakhs and crores as fees and contributions, do not respect the principles of merit and representation, and are characterised by a serious shortage of faculty and clinical material. It would be naive to expect a MBBS doctor who purchased entry to a medical college at great cost to provide health care without extracting a reasonable return on investment.
This is in sync with the government’s strategy of promoting corporate hospital care, which is almost entirely tertiary and higher, as the role model to medical students. This care is beyond the reach of 95% of Indians. Unfortunately, medical education is going the way of private engineering education in India—it is becoming a solitary obsession with numbers, which results in the production of zombie professionals.
The National Medical Commission (NMC) and its earlier incarnations were exclusively focused on the infrastructure and allied hardware that had been arbitrarily defined as essential for setting up new medical colleges. The operating system, the software, and its periodic upgrades, which together define any functional technological application, especially in a vocation that deals with life and death of human beings, received little attention. This should have included having empowered teaching faculty endowed with appropriate pedagogical skills, a commitment to preparing competent healers for India’s vast population, and a programme of action to systematically upgrade their skills and knowledge. It should also have involved conducting research and pushing the boundaries of medical science to solve India’s unique health challenges.
But none of this has received adequate attention from either the governing establishment or the medical profession. The faux belief that digital tools are a substitute for a teacher-mentor relationship is being perpetuated without the realisation that knowledge is a relatively minor component of what makes a doctor. It is the application of knowledge with skills and aptitude that make a good healthcare professional.
[A]ny effort to reform the intent and content of medical education must be done in tandem with the transformation of nursing and paramedical education.
It is pertinent to ask if the government’s strategy will enable the medical education establishment to prepare health professionals who can deliver universal healthcare to all the country’s citizens. The unambiguous answer is that today’s medical education does not prepare medical students to effectively manage contemporary health challenges, let alone emerging ones. The system is at best designed to produce doctors for the tertiary healthcare and not for the primary and secondary healthcare systems.
Way forward
Against this background, the need of the hour is not incremental change, but a comprehensive overhaul of medical education that aligns it with the needs of the country, the goal of universal healthcare, and the spirit of the SDGs.
First and foremost, any effort to reform the intent and content of medical education must be done in tandem with the transformation of nursing and paramedical education. The central and state governments, health universities, professional associations, and civil society must come together to explore the options available to achieve this.
The training of health professionals must be embedded within the strategic framework for achieving quality universal healthcare. Their knowledge, skills, competencies, and values must be geared towards providing universal healthcare in India. For this to happen, all political parties must reach a consensus and affirm their commitment to universal healthcare as a fundamental right. This must be incorporated in the Constitution with a legislative framework for operationalising it.
The NMC could be reconfigured as a national health university along the lines of the University Grants Commission with the mandate to lead, guide, monitor, and direct all matters related to the training of human resources for the country’s health system. It must be endowed with the responsibility of educating all health professionals, including doctors, nurses, pharmacists, paramedical professionals, dental surgeons, and AYUSH professionals.
To ensure uniform standards of health education that are in harmony with the context in each state, every state must have a health university as a single entity responsible for the education of all health professionals, that must include those in the public and private domain. The university must be empowered to not only conduct examinations and award degrees but also to design syllabi and training curriculum, to periodically upgrade the pedagogical skills of the faculty, and to enforce compliance with the national and state-specific standards in all medical, nursing, dental, para-medical colleges.
There is an urgent need for a national, state, and district health human resources strategy stretching up to 2050, and a five-year plan that determines what human resources are needed in each location to achieve universal health coverage by 2030 and to sustain it thereafter. The establishment of colleges to train health professionals and the quality of their training must flow from this strategy.
[B]oth the paucity of medical faculty and the sub-optimal pedagogical skills of the existing faculty need remedial action. Experienced specialists must be enlisted as visiting faculty and retired professors who have a passion for teaching must be contracted as emeritus professors to fill gaps in the interim.
This would entail a freeze on new medical colleges and adding additional seats in states that have reached the threshold of 10 doctors per 10,000 population. It would also need a complete overhaul of the guidelines for setting up medical colleges, and this should include not just infrastructure, but also the teaching faculty that should include applied sociology, economics, ethics, etc.
Both the paucity of medical faculty and the sub-optimal pedagogical skills of the existing faculty need remedial action. Experienced specialists must be enlisted as visiting faculty and retired professors who have a passion for teaching must be contracted as emeritus professors to fill gaps in the interim. Continuous faculty training is essential in not only teaching skills, but also communication, patient management, hospital management, and teamwork, which includes treating nurses and other health professionals on equal terms. All this requires a residential system for both students and the faculty, who will have to be provided with appropriate incentives, both financial and non-financial.
The medical education curriculum now divided into pre-clinical and clinical years needs to be restructured with a focus on disease prevention, health promotion, clinical management, and rehabilitation, with an emphasis on continuum of care. Public health needs to be an integral part of everybody’s education alongside field work in primary or secondary healthcare centres. The objective of MBBS education must be to produce a community physician with the knowledge, skills, and competencies to manage primary and secondary health challenges. Sociology and the economics of health management must be an integral part of the curriculum, in addition to primary health centre and hospital management.
The one-year internship, called house surgency, which is the period during which new doctors are expected to learn to apply their knowledge, is now being used by most to study for the post-graduate entrance examination. Therefore, the house surgency must be increased to two years with the second year devoted to a speciality of the student’s choice. The new doctors must be paid a fair and reasonable financial compensation during this period. The NMC’s proposed national exit exam is welcome as it could help bring about some uniformity.
There is a need for introducing a postgraduate course in family medicine, like the UK’s General Practice (GP), giving every MBBS graduate an opportunity to acquire a postgraduate degree. This would ensure that every physician is skilled in primary and secondary healthcare and has a strong foundation in maternal and child health, and nutrition, in addition to knowing how to work in a referral services system. With the gatekeeping system in place, patients would be required to visit a primary care physician to authorise access to specialty care. It would ensure continuum-of-care and reduce the cost of tertiary care.
Medicine is a rapidly evolving science with constant technological innovations, and this must be reckoned with while preparing doctors for the 21st century. Research that fosters innovation and enables the improved application of knowledge and skills must be sine qua non for modern medical practitioners.
[T]raining as a doctor has to be rooted in the guru-shishya tradition, where the mentor transfers not just the art and science of medical knowledge and skills, but also the values and ethics that are fundamental to using them.
Transforming medical education alone is unlikely to help realise the goal of universal healthcare unless there is a concurrent restructuring of nursing, paramedical, and pharmacy courses. Reforming nursing education and empowering nursing practice requires adapting principles that have been widely practiced in the developed world and closer home at the Christian Medical College, Vellore. A live integrated national registry of health professionals must also be established with a periodic review for accreditation so that all health professionals keep up to date with evolving knowledge and skills.
Another important matter relates to the AYUSH disciplines that attract more than 30,000 students every year. While the tradition and practice of these systems are old, they have not evolved in accordance with the principles of empirical scrutiny. Moreover, AYUSH systems tend to treat individuals but ignore the larger community perspective. There is a need for subjecting AYUSH disciplines to the principles of modern scientific scrutiny as a long-term goal. In the short term, their curriculum should include public health training with a focus on preventive and promotive healthcare.
Being a doctor, or for that matter any health professional, is not just another vocation. It is a calling, a mission, a lifetime commitment to healing not just sick individuals but large societies. More importantly, training as a doctor is rooted in the guru-shishya tradition, where the mentor transfers not just the art and science of medical knowledge and skills, but also the values and ethics that are fundamental to their application. Medical education with an ethical foundation has to be embedded in the quest for scientific excellence. This will remain a distant dream if insatiable greed continues to drive private medical education and its practice.
India can be a developed nation when it celebrates 100 years of independence in 2047. This would become a reality only if every Indian is healthy and has access to accessible, affordable, and acceptable healthcare. Those equipping and managing the health system must be passionately committed to the physical and mental well-being of every Indian. Let’s hope and wish that such a dream will be realised.
P.V. Ramesh is a physician and a former civil servant. He has been principal health secretary of Andhra Pradesh, vice-chancellor of AP Health University, UNFPA country representative to Afghanistan, and head of UNFPA global programming for security imperilled regions.